Wisdom Tooth
- Home
- Wisdom Tooth
Wisdom Tooth
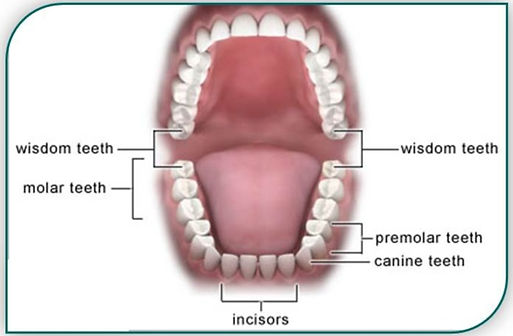
1.Where are my wisdom teeth?
Wisdom teeth are the teeth at the back of your mouth. Wisdom teeth are also known as the third molars. They are usually the last adult teeth to come through the gum and usually appear between 17 and 21 years of age.
2. Why do my wisdom teeth need removing?
Your wisdom teeth may need removing if there is not enough room in your mouth for your wisdom teeth to take their best position. These wisdom teeth aresometimes called “impacted” teeth. All or most of thewisdom tooth may stay below the surface of the gum.Sometimes they may stay deep inside the jaw bone.

Problems due to impacted wisdom teeth may include:
- infected gums
- squashing of the wisdom tooth and the second molar leading to tooth decay of both teeth and/or damage to the second molar
- formation of an unwanted sac of fluid (cyst) which causes damage to the jaw bone, nearby teeth, and, rarely, tumours
- a weakness in the lower jaw which may result in the jaw breaking when a strong force is applied (e.g. in sport or eating hard foods).
3. What happens during removal of my wisdom teeth?
Removal of a wisdom tooth is a minor surgical procedure:
- The tooth and surrounding area will be numbed by anaesthetic.
- You may also be given a sedative medicine to help control any anxiety, if you are nervous.
- Once the area around the tooth is numb, the tooth may need to be uncovered by lifting back the gum or sometimes the gum may need to be cut. Occasionally the dental practitioner/oral surgeon may need to remove some bone surrounding the wisdom tooth.
- The tooth is loosened with movements and pressure. This may require the use of a tooth drill to cut the tooth into two or more pieces.
- The tooth is then removed.
- Stitches may be required and will normally dissolve after 5 days.
- New bone will begin to fill the hole over the next 6 to 8 weeks.
- Removing wisdom teeth may need more than one visit to the dental practitioner or oral surgeon.
4. Will I need an anaesthetic?
- You may need someone to drive you home if you have been given an anaesthetic or sedative. This will be discussed before your procedure.
5. What should I expect after my wisdom teeth are removed?
- You may need someone to drive you home if you have been given an anaesthetic or sedative. This will be discussed before your procedure.
- Pain is common for the first two days. Pain relief tablets may be bought over the counter at a pharmacy. If you need stronger pain control, please discuss this with your dental practitioner/doctor.
- Swelling and puffiness of cheeks which should be gone by 5 days after the procedure.
- Bruising and discolouration below the jaw.
- It may be a over a week before the mouth can be opened widely with comfort. This is because the jaw muscles become tight following surgery.
-
To take up to 4 days off work:
- rest quietly at home
- eat soft, nutritious foods such as soft boiled eggs, finely chopped meat or cheese, custards, milk, soup or fruit juice for several days.
- Healing usually occurs quickly without complications. Problems may arise because the mouth must be used for eating and speaking while healing is taking place. The mouth naturally contains many bacteria which may increase the risk of infection in the wound.
- There may be slight bleeding which is just enough to discolour the saliva for a few hours. There should be continual improvement until healing is complete.
6. What are the specific risks of removal of my wisdom teeth?
The wound normally heals within 2 weeks. Complications may prolong healing.
Common risks and complications include:
-
dry socket: occurs when a blood clot does not form in the hole where the tooth was or the blood clot is disrupted:
- the bone underneath will be exposed to air and food
- it can be very painful and lead to an infection, a bad taste and/or odour in your mouth
- it is more likely to occur if you smoke
- infection.
-
bleeding: this is more common if you take one of the many blood thinning medicines (e.g. Aspirin,Warfarin)
- Do not stop these medicines without medical advice
- Ask your GP, surgeon and/or anaesthetist if you should stop taking these medicines before surgery as it may affect your blood clotting
- If you are asked to stop taking a blood thinning medicine before your procedure, ask your doctor when you can restart the blood thinning medicine
- Biting of the numb lip which may cause damage after the teeth have been removed
- nerve damage causing pain or a tingling sensation and numbness in the tongue, lower lip, chin,teeth and gums; this is usually temporary, but can be permanent in some cases
- bone and root fragments remain in the gum/jaw
- damage to nearby teeth
- jaw weakness: the jaw may break during the procedure or during the healing period
- if the upper teeth are close to the sinuses, removal may cause a hole between the mouth and the sinus; this may need further surgery
- jaw necrosis (the jaw bone dying) if you are on certain medications (mainly for osteoporosis—your doctor/dental practitioner will discuss this with you), or if you are receiving radiation to the head and/or neck.
Uncommon risks and complications include:
7. What are the risks of not having my wisdom teeth removed?
There may be consequences if you choose not to have the proposed treatment. Please discuss these with your dental practitioner/oral surgeon (doctor).If you choose not to have the procedure you will not be required to sign a consent form.
8. Who will remove my wisdom teeth?
Your wisdom teeth will be removed by your dental practitioner or a dental student who has had training to undertake the procedure. You will be referred to an oral surgeon if removing the wisdom teeth is expected to be difficult. A doctor who is training to become an oral surgeon may perform your surgery. This doctor will be supervised by an oral surgeon and according to professional guidelines.
9. Can I help prevent complications following removal of my wisdom teeth?
You can help to prevent complications such as pain, swelling, infection and bleeding by following a few simple rules.
Do not:
- Bite or suck a numb lip, cheek or tongue, as you may injure yourself
- Smoke or drink alcohol for at least 24 hours as it may delay healing
- Place fingers, pencils or any other object in the mouth (this is to avoid injury and/or infection)
- Lie down flat: you can relax but keep the head elevated to decrease the risk of bleeding
- Be too active for about 24 hours
- Rinse your mouth for about 24 hours:
- After the first 24 hours, ensure your mouth is rinsed gently after meals
- Half a teaspoon of table salt dissolved in a glass of lukewarm water is an effective mouth rinse.
10. What if complications arise after my wisdom teeth are removed?
The most common complications are pain, swelling, infection and bleeding.
- Pain:
- Swelling:
- Infection:
- Temporary numbness:
- Bleeding:
- Dry socket (refer to Section 6):
control moderate pain by taking paracetamol. Take as directed and do not apply the drug to the wound itself. If the pain persists or worsens, return to the surgery/dental clinic where you were treated. In most cases, pain can be controlled quickly.
some swelling or difficulty in opening your mouth is common but it should begin to subside after a day or two. If swelling persists or becomes worse, return to the dental clinic where you were treated.
continued pain, swelling, redness or a raised temperature may mean there is an infection present. This is usually treated with antibiotics. If you suspect an infection, return to the dental clinic where you were treated for advice.
can occur due to the irritation of the nerves during the extraction. It is usually only temporary and should return to normal within a few days. Seek advice from the dental clinic you attended if numbness persists.
continued bleeding is not normal. If your mouth is bleeding continuously, remove any excessive blood clots from the mouth as a first step. Then apply a clean and damp rolled bandage or small folded handkerchief to the wound. Keep the cloth in place by applying pressure or firmly closing the jaws around it. Sit down and main pressure for at least 10 minutes.If the bleeding cannot be stopped using this method, telephone the surgery where you were treated for advice.
A dry socket needs to be treated as soon as possible.
More information
How To Know That Dental Filling Is Loose?
Objectively innovate empowered manufactured products whereas parallel platforms. Holisticly predominate extensible testing procedures for reliable.
How To Know That Dental Filling Is Loose?
Objectively innovate empowered manufactured products whereas parallel platforms. Holisticly predominate extensible testing procedures for reliable.